Coronaviruses are a group of viruses that are known to cause mild to severe diseases in animals and humans. A few of the Coronaviruses are known to cause severe respiratory infections in humans, of which Severe Acute Respiratory Syndrome (SARS-2003), Middle East Respiratory Syndrome (MERS-2012) were detected in the past.
A more recent outbreak of Coronavirus called the Novel Coronavirus (SARS-CoV-2) has upsurged pandemically and is spreading throughout the world since its outbreak in December 2019, from the Chinese city of Wuhan.
Coronaviruses were considered to be harmless entities until the SARS-CoV outbreak in 2003. The origin of this virus remains debated but repeatedly marked and confirmed to be contained in bats. The Novel Coronavirus (SARS-CoV-2), also doesn’t have a solid source to mention and is assumed to have spread from a sea-food market in Wuhan, where a variety of animals were supplied as food, revealing its proximity being of animal origin.
Classification and Structure
These viruses belong to the family Coronaviridae and Subfamily Orthocoronaviridae.
Four genera of these coronaviruses, namely Alpha-, Beta-, Gamma- and Delta- are classified depending on their origin, antigenicity, and differences in the surface protein.
Sequence analysis has revealed that the Novel Coronavirus(SARS-CoV-2) including SARS-CoV and MERS-CoV are Beta-coronaviruses, and posses marked similarities suggesting them of the same animal origin.
The Coronaviruses are enveloped and have a spherical shape, with a diameter of approximately 120 nm. The viral envelope has surface projections resembling the solar corona that is anchored to the envelope together with the lipid bilayer. Members of beta-coronaviruses also display shorter projections of Hemagglutinin Esterase (HE) protruded from their envelopes.
According to the Centers for Disease Control and Prevention (CDC), the most common coronaviruses identified are:
- 229E (alpha Coronavirus)
- NL63 (alpha Coronavirus)
- OC43 (beta Coronavirus)
- HKU1 (beta Coronavirus)
The severe disease-causing viruses from the Coronavirus family,
- MERS-CoV (beta Coronavirus)
- SARS-CoV (beta Coronavirus)
- SARS-CoV-2 / The Novel Coronavirus (beta Coronavirus)
Molecular Genomics
Coronaviruses contain a positive-stranded RNA genome of approximate size between 26kb to 34 kb and contain 6–11 Open Reading Frames (ORFs). This genome is adhered to the capsid present inside the envelope along with N-protein.
On the genome level, the novel coronavirus is 96% identical to the Bat Coronavirus.
Specifically, the genome size of SARS-CoV-2 as estimated from three isolated strains is on average 29.8kb. It contains 14 ORF’s that encodes for 27 proteins. The first ORF constitutes about approx. 67% of the entire genome and encodes many non-structural proteins. The genes orf1ab and orf1a near the 5'-terminus encode pp1ab and pp1a respectively, which comprises 15 nsps’ (Non-structural polyproteins) including nsp1 to nsp10 and nsp12 to nsp16.
Initially, the translation of this ORF encodes a long-chain polyprotein which is cleaved by a protease derived from the polyprotein itself. These smaller proteins are known to form a multi-protein structure called the Replicase-Transcriptase Complex (RTC) which functions on its entirety for replication and transcription of the viral genome. It has a primary sub protein, the RNA-dependent RNA-polymerase directly involved in the function of replication and transcription.

Other ORF’s in the genome encodes the accessory and structural proteins. The accessory proteins assist the RTC complex in the replication and transcription process. Near the 3′-terminus of Novel coronaviral genome, four structural proteins (S, E, M, and N) and eight accessory proteins (3a, 3b, p6, 7a, 7b, 8b, 9b, and orf14) are mapped. These four structural proteins are — the Nucleocapsid Protein (N), Spike Protein (S), Small membrane protein (E) and Membrane glycoprotein (M).
The gene for Hemagglutinin Esterase (HE) additionally is present in the beta-Coronaviruses (HCoV‐OC43 and HKU1)

The plus-strand RNA of the viral genome is used for the synthesis of negative-strand genomic RNA by the RTC, which is then followed by the synthesis of positive-strand genomic RNA.
Transmission and Infection:
Human to human transmission is common for the COVID-19 and the virus is transmitted primarily through the respiratory route.
Any human being infected with COVID-19 virion exhales tiny droplets or packets of fluid from nose and mouth while breathing, sneezing or coughing which contain the virus particles. As soon as those infectious droplets are airborne, they land on the skin surfaces of uninfected persons. These surfaces are often touched by hands that carry the virus swiftly to the eyes, nose or mouth.
Those infectious droplets can also be inhaled by healthy persons directly from the air. Unlike the bacterial spores, there is no evidence that the droplets can be carried long distances by air to cause infections, but the possibility still exists. Health professionals advise keeping a distance of at least 3 meters when dealing with a COVID-19 patient.
Both phylogenetically and in the infection mechanism, the novel Coronavirus (SARS-CoV-2) is more identical to the SARS-CoV. SARS infects the type-2 pneumocytes and ciliated bronchial epithelial cells in the lungs mediated by Angiotensin-Converting Enzyme2 (ACE2) as the host receptor. This receptor facilitates adherence and penetration of the target cells.
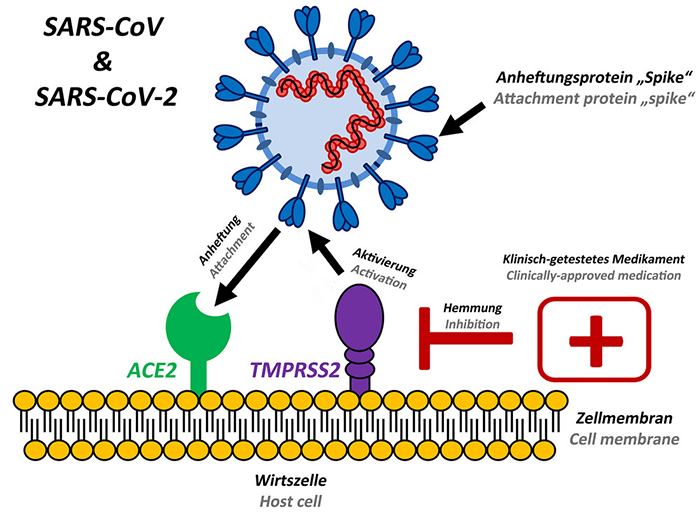
Adult humans express an enzyme ACE2 (Angiotensin Converting Enzyme 2), an exopeptidase to convert a wide array of enzymes to regulate the cardiac function. The infection of novel Coronavirus (SARS-CoV-2) is also mediated by the same receptor for penetrating the lung’s alveolar epithelial cells.
Other coronaviruses such as MERS-CoV use dipeptidyl peptidase 4 (DPP4), a membrane glycoprotein to infect the target cells.
Symptoms and Viral Pneumonia
The most common symptoms associated with COVID-19 include fever, cough, and tiredness.
Of them, some also experience flu-like symptoms like runny nose, sore throat, aches, nasal congestion and sometimes, diarrhea. The symptoms appear to begin gradually, and with mild beginnings. A fraction of patients, however, do not develop any symptoms even when affected (asymptomatic).
Without symptoms, these infected beings remain as the silent carriers of the disease.
Statistically, the clinical symptoms of the infection of COVID-19 by the end of February 2020 revealed (approx.):
- Fever — In 89% of the patients
- Cough — In 68% of the patients
- Difficulty Breathing — 55% of the patients
- Fatigue — 44% of the patients
Following the infection symptoms, approximately 75% of the patients develop Pneumonia in the second or third week of the symptomatic infection. Pneumonia involved the following clinical manifestations:
- Decreased Oxygen Saturation
- Blood gas deviations
- Ground Glass Opacity in Chest CT — 54% of the patients (a confirmatory manifestation)
- Alveolar exudates and interlobular movement
- Lymphocytopenia (decreased lymphocytes) in 83% of the patients
- Increased CRP and Pro-inflammatory Cytokines.
The infection spread rate from early cases demonstrated the epidemic doubled among affected individuals in every seven days. On average, every patient spread infection to 2.2 other individuals.
Treatment Approaches
An array of drugs and methods are being tested and researched for a one-stop solution to the recent outbreak of COVID-19. In general, the treatment strategies for this novel disease can be functionally categorized into the following approaches.
Genetically Engineered Cells
Genetically engineered cells specifically target the whole virion particle or the infected cell for destruction. Immunotherapy using genetically engineered T-cells having shown promises for cancer and can also be used clear virus particles rapidly from the infected host. The cells engineered for targeting the virion can also trigger a protective immune response, forcing the virion to be killed by the host defense mechanism, or induce the infected cell to die by apoptotic triggers.
Moreover, this form of treatment might take a while for research and testing. Since time is the only constraint in the pandemic outbreak of COVID-19, this approach might not be able to give its results ahead in real-time.
Immunization/ Development of Vaccine
A vaccine is usually a biological substance that triggers the production of antibodies against a specific antigen in the host. Antibodies are the mediators of immune response that bind and target the infectious particles such as bacteria, viruses, and other particles for destruction by the immune system of the host. Usually, vaccines are derived by utilizing non-infectious but antigenic property in an organism that can trigger a massive immune response in the host body to produce antibodies. B-cells are the specialized white blood cells that produce the antibodies when signaled by an array of immune mechanisms.
However, the development of vaccines can take years to be designed and trialed for its effects before deploying into clinical practice.
Medicine Therapy
There are no medical preparations to date that have proven specifically to control the novel Coronavirus (SARS-CoV-2).
The medicine therapy also cannot produce instant results for the pandemic disease, as the research and development can take decades before the drug is approved for general use. However, an already existing drug can be deployed for its possible efficacy against COVID-19. Combined antiviral therapies and drugs prepared by small structural changes can be produced with relative ease and less time.
The use of already existing drugs thus can be the best alternative to deal with the novel disease in the state of urgency.
Studies have shown the drugs like Baricitinib (AAK1 and Janus kinase inhibitor), remdesivir (adenosine analog that acts as a viral protein inhibitor), Chloroquine (increases the endosomal pH affecting virus-cell fusion), combined therapies of lopinavir and ritonavir, mesenchymal stem cell treatment, darunavir plus cobicistat, hydroxychloroquine, methylprednisolone, and others have shown promises for defeating the viral infections or at least in slowing it down.
Preventive measures
Prevention is better than cure and something is by far better than nothing. The rapid spread of the CoVID-19 has alarmed the world and is testing the medical systems throughout. Different practices for treating and isolation of the infected are implemented to halt the spreading virus.
By the time this article was written, the disease has already been confirmed in 147 countries around the world, with 147,838 people affected. The death toll has reached 5,539 (3.7%) and the surge of infections is most active in Europe(Italy) and has entered Africa.

The results are from the real-time information system for Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU).
As advised by the WHO, the safety measures are intended to reduce the chances of being infected or spreading the COVID-19, has the following objectives.
Maintain social distance
- Maintain at least 1 meter (3 feet) distance between yourself and anyone who is coughing or sneezing.
Maintain Personal hygiene
- Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
- Avoid touching eyes, nose and mouth.
- Cover your mouth and nose with your bent elbow or tissue when you cough or sneeze.
Don’t ignore the signs
- Common cold and CoVID-19 might show similar symptoms, but the later one can turn severe with time. If you have a fever, cough and difficulty breathing, seek medical attention.
- Keep up to date on the latest COVID-19 hotspots (cities or local areas where COVID-19 is spreading widely).
…………………………………Stay safe………………………………
Sources:
Habibzadeh, P., & Stoneman, E. K. (2020). The Novel Coronavirus: A Bird’s Eye View. The international journal of occupational and environmental medicine, 11(2), 65.
Velavan, T. P., & Meyer, C. G. (2020). The COVID‐19 epidemic. Tropical Medicine & International Health.
Yang, Y., Shang, W., & Rao, X. (2020). Facing the COVID‐19 outbreak: What should we know and what could we do?. Journal of Medical Virology.
Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., … & Du, B. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine.
Wu, A., Peng, Y., Huang, B., Ding, X., Wang, X., Niu, P., … & Sheng, J. (2020). Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host & Microbe.


Post a Comment